以生肽共軛修飾之脂雙層基質進行磷酸鈣二維生物材料之鉅觀與奈米尺度操控
2D biomaterials of Calcium Phosphate Nanocomposite with control macro and nanoscale morphology via Peptide Conjugated Supported Lipid Bilayer
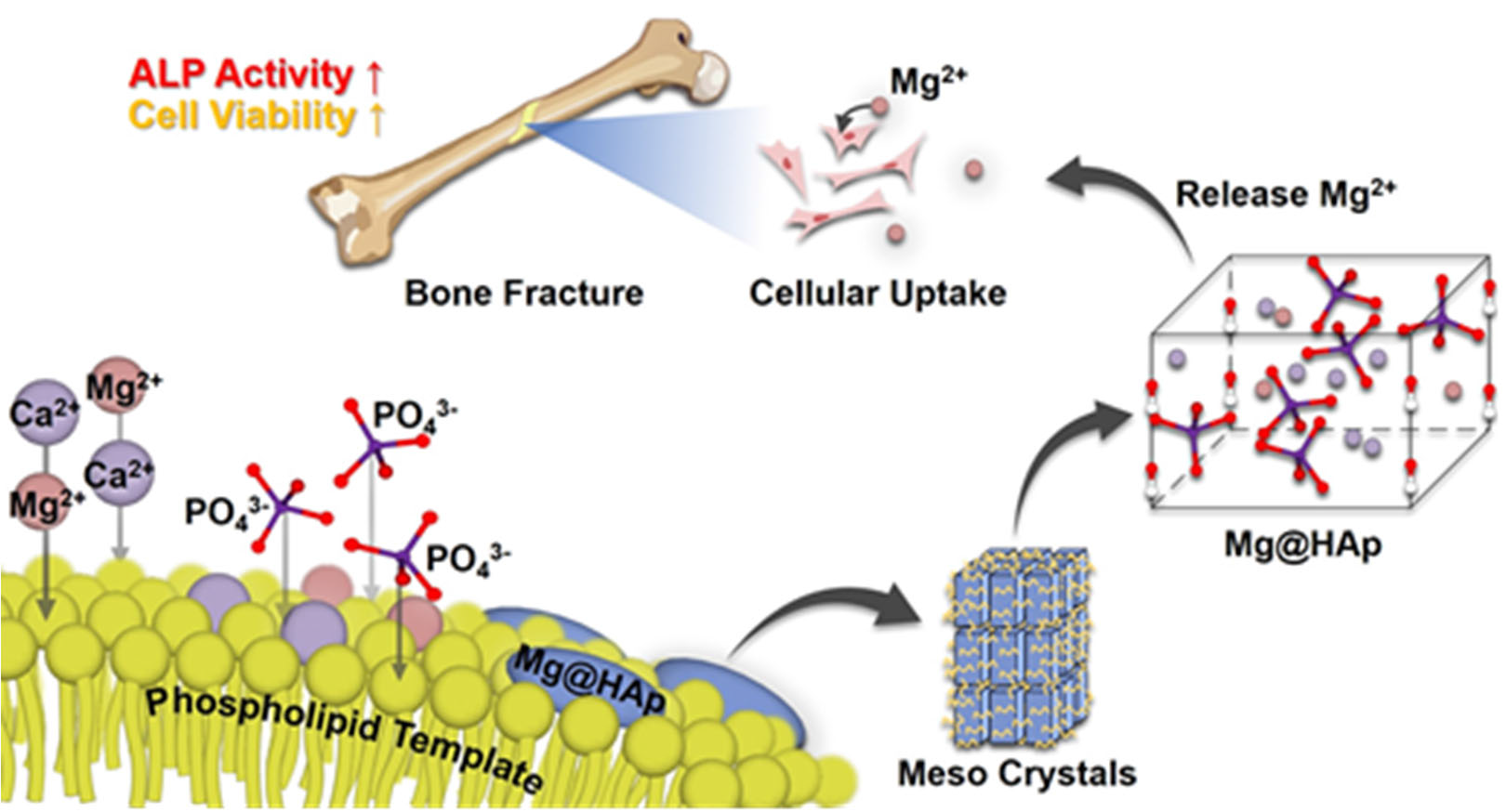
本計畫藉由仿生物礦化的方式,發展了一個以磷脂質為模板的含鎂磷酸鈣合成方法,經過X 射線繞射以後發現即使我們採用相對溫和的合成條件(37 °C 對比傳統的高溫燒結),還是可以獲得良好的氫氧基磷灰石(Hydroxyapatite, HAp)晶相。同時,我們發現磷脂質的存在使得磷酸鈣晶體中,更多的鈣離子可以被鎂離子取代。藉由實驗的設計,我們推測磷脂質的兩性離子特性(Zwitterionic)可以在合成時吸附鎂離子,幫助鎂離子進入磷酸鈣的晶格。而霍式轉換紅外光譜儀(FT-IR)的結果則指出磷脂質無法被完全的從含鎂磷酸鈣移除。之後我們由穿透式電子顯微鏡的影像得知柱狀的磷酸鈣晶體在磷脂質的纏繞下形成了介晶(Mesocrystal)結構,不僅是排列方向一致,有機與無機交錯的排列就如同人體骨骼的微結構一般。
接著我們對含鎂磷酸鈣進行四週的降解實驗後得出了28.06 wt%的降解率,並且在對類骨母細胞MG-63系的實驗中得出大約會有0.89 wt%的鎂離子被釋出,而MG-63 細胞系在攝入磷酸鈣的降解物後,三天內細胞活性就可以提升到127%,ALP 濃度也提高到了222 %,根據文獻,雖然機制尚不清楚,但骨母細胞的分化行為總會伴隨著ALP 濃度的提高,此結果可以說明我們所發展之含鎂磷酸鈣具有促進骨分化之能力,是非常具有潛力的骨治療材料。
By mimicking the biomineralization process, we successfully developed a magnesium-loaded calcium phosphate material. The X-Ray Diffraction patterns indicated that the crystal phase of our material is Mg-loaded hydroxyapatite (Mg@HAp). We found that even if we applied mild synthesis conditions, a good crystallinity of HAp could still be obtained. At the same time, the presence of phospholipids increases the amount of magnesium substitutions in the HAp lattice, which is controllable from 1.44 to 10.64 wt%. To find out the mechanism, we designed an experiment and finally hypothesized that the zwitterionic nature of phospholipid makes it capable of adsorbing magnesium ions during synthesis and helps magnesium ions enter the HAp lattice. It should be noted that the phospholipid could not be completely removed from Mg@HAp according to the Fourier Transform Infrared (FT-IR) Spectra. Transmission Electron Microscope (TEM) images of our Mg@HAp showed that microcrystalline HAp crystals formed a mesocrystal structure entangled by the phospholipids. The formation of the orderly crystal alignment is attributed to the phospholipid organic matrix’s presence.
To know whether our material is suitable for bone fracture treatment, we have done the in vitro degradation test and cell culture experiments with osteoblast-liked cell MG-63. The degradation rate for Mg@HAp could be controlled in a range of 9.71 to 28.06 % in 4 weeks in the phosphate buffer saline. And the Mg content is the primary factor of HAp’s degradation rate, whereas increasing Mg content resulted in a higher degradation rate. For the cell culture experiments, there were 0.89 wt% Mg ions released from Mg@HAp, leading to 127% cellular viability and 222% ALP concentration after three days of culture.
We concluded that the presence of high Mg and addition of phospholipid in HAp are beneficial to cellular proliferation and differentiation of osteoblasts, and the release of Mg ions is an important factor as well. All these results indicate that Mg@HAp is a potential biomaterial for bone fracture treatment.